Prednisone stands out as a powerful option for managing inflammation in various medical conditions. This synthetic corticosteroid mimics the effects of hormones produced by the adrenal glands, effectively reducing swelling and suppressing immune responses. For those dealing with conditions such as arthritis, asthma, or autoimmune disorders, prednisone can offer significant relief and improvement in quality of life.
When considering prednisone, dosage and duration are key factors. Typically prescribed in low doses, physicians tailor treatment plans based on individual needs and response to therapy. Starting with a higher dose and tapering down gradually often maximizes benefits while minimizing side effects. Understanding potential side effects is essential; common issues include weight gain, mood changes, and increased blood sugar levels.
Monitoring is crucial during treatment. Regular check-ups help assess the effectiveness of the medication and any adverse effects. Patients are encouraged to communicate openly with their healthcare provider about their progress and any concerns they may have. By staying informed and proactive, the use of prednisone can be safe and beneficial for managing inflammation effectively.
- Use of Prednisone for Inflammation
- Dosing and Administration
- Potential Side Effects
- Understanding Prednisone: What It Is and How It Works
- Mechanism of Action
- Common Uses and Benefits
- Common Inflammatory Conditions Treated with Prednisone
- Asthma and Allergic Reactions
- Autoimmune Disorders
- Dosage Guidelines for Prednisone Use in Inflammation
- Adjustment and Tapering
- Specific Conditions and Considerations
- Benefits of Prednisone in Managing Inflammatory Symptoms
- Rapid Symptom Relief
- Wide Range of Applications
- Adaptability of Treatment
- Prevention of Flare-Ups
- Potential Side Effects and Risks of Long-Term Prednisone Use
- Strategies to Minimize Side Effects While Taking Prednisone
- Regular Monitoring and Communication
- Gradual Dose Adjustment
- When to Consult a Doctor About Prednisone Treatment
- Monitoring Dosage and Duration
- Interactions with Other Medications
Use of Prednisone for Inflammation
Prednisone rapidly reduces inflammation and is commonly prescribed for a variety of conditions, including arthritis, asthma, and autoimmune disorders. To maximize its benefits, adhere to your healthcare provider’s dosage instructions.
Dosing and Administration
- Start with a low dose as recommended by a doctor.
- Gradually adjust the dose based on your response and any side effects.
- Do not abruptly stop the medication to prevent withdrawal symptoms; tapering may be necessary.
Potential Side Effects
While prednisone is generally effective, some individuals experience side effects. Common issues include:
- Increased appetite, leading to weight gain.
- Elevated blood sugar levels, particularly in those with diabetes.
- Sleep disturbances and mood changes.
- Long-term use may lead to osteoporosis; discuss bone health with your doctor.
Monitoring and follow-up appointments can help manage any adverse reactions. Make sure to inform your healthcare provider about all medications you are taking to avoid interactions. Prednisone can significantly improve quality of life by effectively managing inflammation, but continuous evaluation of its use is crucial for safety and efficacy.
Understanding Prednisone: What It Is and How It Works
Prednisone serves as a powerful anti-inflammatory medication commonly used to manage various autoimmune conditions and inflammatory disorders. It mimics the effects of cortisol, a hormone produced by the adrenal glands, helping to reduce inflammation and suppress the immune response.
Mechanism of Action
Upon administration, prednisone converts into prednisolone in the liver. This active form binds to glucocorticoid receptors, leading to a cascade of biological effects that inhibit the production of inflammatory substances, such as cytokines and prostaglandins. This process not only alleviates pain and swelling but also enhances the body’s tolerance to stress.
Common Uses and Benefits
Healthcare providers often prescribe prednisone for conditions like arthritis, asthma, and inflammatory bowel disease. It can significantly improve symptoms, increase mobility, and enhance the overall quality of life. Dosage typically starts low and adjusts based on response, ensuring the optimal balance between benefits and potential side effects.
Common Inflammatory Conditions Treated with Prednisone
Prednisone effectively addresses a variety of inflammatory conditions. Rheumatoid arthritis is one of the primary disorders where this corticosteroid provides relief from joint pain and swelling. Patients often experience significant improvement in mobility and a reduction in disease symptoms after starting treatment.
Asthma and Allergic Reactions
Asthma management frequently includes prednisone during exacerbations. This drug reduces airway inflammation, allowing for easier breathing. Additionally, it helps control severe allergic reactions by suppressing the immune system’s response, minimizing symptoms like swelling and hives.
Autoimmune Disorders
Systemic lupus erythematosus and multiple sclerosis are autoimmune diseases where prednisone plays a key role. In lupus, it helps manage flares by reducing inflammation throughout the body. In multiple sclerosis, prednisone alleviates acute symptoms during relapses, aiding recovery and enhancing patient comfort.
Dosage Guidelines for Prednisone Use in Inflammation
Doctors typically recommend an initial dose of prednisone ranging from 5 mg to 60 mg per day, depending on the severity of the inflammation and individual patient factors. Start with a lower dose for mild conditions, and adjust as necessary based on response and side effects.
Adjustment and Tapering
Monitor patients closely for therapeutic response and adverse effects. If significant improvement occurs, consider gradually reducing the dose. Tapering is crucial to prevent adrenal insufficiency. A common tapering schedule reduces the daily dosage by 5-10 mg every one to two weeks, depending on the patient’s status and duration of therapy.
Specific Conditions and Considerations
For conditions like rheumatoid arthritis or lupus, higher doses around 20 mg to 40 mg may be warranted, especially during flare-ups. In acute cases, short courses of high doses might be prescribed, followed by a taper. Renal or hepatic impairment may necessitate dosage adjustments. Always consult with a healthcare provider to personalize the treatment plan and dosage.
Benefits of Prednisone in Managing Inflammatory Symptoms
Prednisone efficiently reduces inflammation and alleviates symptoms associated with various conditions. It provides rapid relief, making it a preferred choice for many healthcare providers.
Rapid Symptom Relief
Patients often experience significant improvement in a matter of days. Prednisone quickly decreases pain, swelling, and redness, allowing individuals to regain their functionality and comfort almost immediately.
Wide Range of Applications
- Prednisone treats autoimmune diseases such as lupus and rheumatoid arthritis effectively.
- It manages respiratory conditions like asthma and COPD by decreasing airway inflammation.
- In skin conditions, such as dermatitis, it alleviates itching and irritation.
Customized dosing allows adjustment based on individual response, optimizing the therapeutic impact.
Adaptability of Treatment
Healthcare professionals frequently utilize prednisone in varying treatment plans, either as a standalone therapy or in combination with other medications. This flexibility enhances its role in comprehensive treatment strategies.
Prevention of Flare-Ups
Long-term use, under careful supervision, can help prevent future inflammatory flare-ups, contributing to sustained patient health and well-being.
- Reduce healthcare costs associated with hospital visits.
- Improve quality of life through constant management of symptoms.
Prednisone remains a valuable tool in the medical arsenal against inflammation, offering immediate and effective symptom management in various inflammatory conditions.
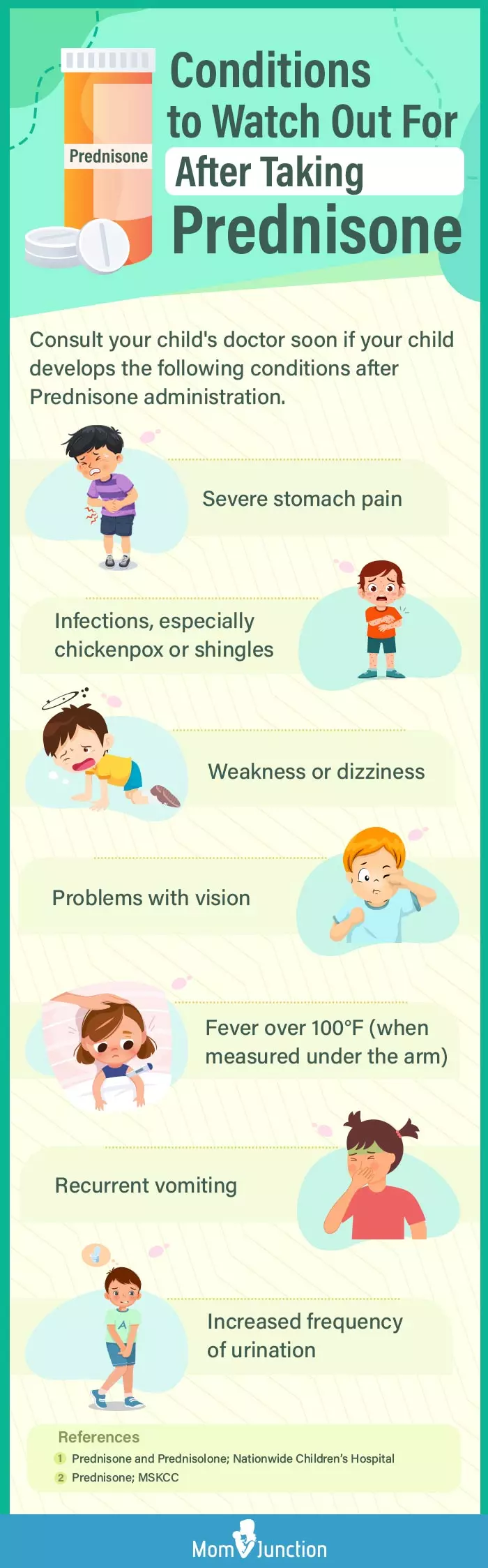
Potential Side Effects and Risks of Long-Term Prednisone Use
Long-term use of prednisone may lead to several side effects and health risks. Awareness of these potential issues is key for patients and healthcare providers. Regular monitoring can prevent or mitigate adverse effects.
Weight gain often occurs with long-term prednisone therapy due to increased appetite and changes in fat distribution. Engaging in regular physical activity and adhering to a balanced diet can help manage weight.
Bone density loss is another significant concern. Prednisone can lead to osteoporosis, making bones more fragile and prone to fractures. Patients should consider calcium and vitamin D supplementation, alongside weight-bearing exercises, to support bone health.
Increased blood sugar levels represent a risk for diabetes development. Regular blood sugar monitoring is essential for individuals on long-term steroids. Dietary adjustments may aid in maintaining stable glucose levels.
Gastrointestinal complications, such as gastritis or peptic ulcers, can arise. Taking prednisone with food reduces irritation and lower the risk of these conditions. Healthcare providers may prescribe protective medications like proton pump inhibitors.
Adrenal suppression is another serious side effect. Long-term use can inhibit the body’s cortisol production. Gradual tapering off the medication under medical supervision is critical to allow adrenal function to recover.
Other potential side effects include mood changes, increased risk of infections, and skin problems like thinning or easy bruising. Open communication with healthcare professionals regarding any emerging symptoms is advisable.
| Side Effect | Management Strategy |
|---|---|
| Weight Gain | Exercise, Balanced Diet |
| Bone Density Loss | Calcium/Vitamin D, Weight-Bearing Exercise |
| Increased Blood Sugar | Regular Monitoring, Dietary Adjustments |
| Gastrointestinal Issues | Take with Food, Proton Pump Inhibitors |
| Adrenal Suppression | Gradual Tapering |
| Mood Changes | Regular Check-Ins with Provider |
| Increased Infection Risk | Preventive Measures, Vaccinations |
| Skin Problems | Moisturizers, Gentle Skincare |
Close monitoring and proactive management can help mitigate these risks associated with long-term prednisone use. Consult healthcare professionals regularly to tailor treatment to individual needs.
Strategies to Minimize Side Effects While Taking Prednisone
Maintain a healthy diet rich in fruits, vegetables, and whole grains. This approach helps reduce the risk of weight gain and supports overall health. Consider increasing your intake of potassium through foods like bananas, spinach, and avocados, as prednisone can lower potassium levels.
Stay well-hydrated. Drinking plenty of water helps your body manage fluid retention and reduces swelling. Limit sodium intake to minimize high blood pressure and related issues.
Regular Monitoring and Communication
Schedule regular follow-ups with your healthcare provider. Monitoring blood pressure, blood sugar, and bone density can catch problems early and allow for prompt adjustments to your treatment. Discuss any side effects you experience; adjustments to dosage or alternative medications might be necessary.
Gradual Dose Adjustment
Follow your doctor’s advice on tapering doses when it’s time to stop taking prednisone. This reduces the risk of withdrawal symptoms and helps your body adjust to changing levels of corticosteroids.
Incorporate moderate exercise into your routine. Activities like walking, swimming, or yoga can combat weight gain, boost mood, and strengthen bones. Consult with a healthcare professional before starting any exercise program.
Lastly, practice stress-reducing techniques such as meditation or deep-breathing exercises. These can help mitigate mental and physical side effects, leading to improved overall well-being.
When to Consult a Doctor About Prednisone Treatment
Consult a doctor if you experience severe side effects while taking prednisone. Symptoms such as chest pain, difficulty breathing, or swelling in the face or limbs warrant immediate medical attention. These may indicate an allergic reaction or other serious complications.
If you notice a significant change in mood, such as increased anxiety or depression, reach out to your healthcare provider. Emotional disturbances can occur due to corticosteroid treatment, and adjusting the dosage or switching medications may be necessary.
Monitoring Dosage and Duration
Regular consultations are essential if you are on long-term prednisone treatment. Your doctor should monitor the dosage to minimize risk factors like adrenal insufficiency or osteoporosis. If you’ve been prescribed prednisone for an extended period, discuss potential tapering strategies to safely discontinue the medication.
Interactions with Other Medications
Inform your doctor about all medications you are taking, including over-the-counter drugs and supplements. Certain medications can interact negatively with prednisone, enhancing side effects or diminishing therapeutic efficacy. A healthcare professional can help you manage these interactions effectively.