When faced with bacterial infections, Floxacillin emerges as a reliable choice. This antibiotic excels in treating various conditions caused by susceptible bacteria. Clinicians often prescribe it for skin infections, respiratory tract infections, and some types of gastrointestinal infections.
Floxacillin functions effectively against penicillin-resistant strains of Staphylococcus aureus. For optimal results, it’s crucial to administer the medication exactly as directed by a healthcare professional. Awareness of possible interactions with other medications enhances patient safety.
Monitoring treatment response is equally important. Patients should report any side effects such as allergic reactions or gastrointestinal disturbances to their healthcare provider promptly. Regular follow-ups ensure that the antibiotic continues to be the right fit for the ongoing infection.
- Floxacillin Antibiotics: A Comprehensive Overview
- Mechanism of Action
- Indications and Usage
- Side Effects and Considerations
- Clinical Uses of Floxacillin in Treating Infections
- Skin and Soft Tissue Infections
- Respiratory Tract Infections
- Mechanism of Action and Pharmacokinetics of Floxacillin
- Side Effects and Contraindications of Floxacillin Treatment
- Common Side Effects
- Contraindications
- Guidelines for Prescribing and Dosage Adjustments of Floxacillin
Floxacillin Antibiotics: A Comprehensive Overview
Floxacillin serves as a valuable option for treating various bacterial infections. This antibiotic effectively targets gram-positive bacteria, making it suitable for conditions such as skin infections, septicemia, and respiratory tract infections.
Mechanism of Action
Floxacillin disrupts bacterial cell wall synthesis. It binds to penicillin-binding proteins (PBPs), inhibiting transpeptidation, which is crucial for cell wall integrity. This leads to bacterial lysis and death, effectively eliminating the infection.
Indications and Usage
- Skin and Soft Tissue Infections: Primarily used for infections caused by staphylococci and streptococci.
- Bone Infections: Administered in cases of osteomyelitis.
- Respiratory Infections: Treats pneumonia and other respiratory tract conditions.
Proper dosage is critical for optimal results. Adult dosages typically range from 250 mg to 500 mg every 6 hours, depending on the severity of the infection and patient response.
Side Effects and Considerations
- Gastrointestinal Distress: Possible nausea, vomiting, and diarrhea.
- Allergic Reactions: Monitor for signs of rash or anaphylaxis.
- Resistance: Awareness of resistance patterns in local flora is critical for effective treatment.
Regular follow-ups help assess the effectiveness and adjust treatment as needed. Always consult a healthcare provider before starting or changing any antibiotic regimen.
Clinical Uses of Floxacillin in Treating Infections
Floxacillin is commonly used in treating various bacterial infections, particularly those caused by penicillin-sensitive organisms. This antibiotic effectively targets infections such as skin and soft tissue infections, pneumonia, and septic arthritis. Its ability to combat staphylococci, including penicillin-resistant strains, makes it a valuable option in clinical settings.
Skin and Soft Tissue Infections
Floxacillin is frequently prescribed for skin and soft tissue infections like cellulitis and abscesses. It works well against methicillin-sensitive Staphylococcus aureus (MSSA), which is crucial in managing these conditions. In many cases, clinicians opt for Floxacillin over other antibiotics when there is a high likelihood of staphylococcal infection.
Respiratory Tract Infections
In cases of pneumonia caused by susceptible bacteria, Floxacillin serves as an effective treatment. It demonstrates activity against Streptococcus pneumoniae, a common pathogen in respiratory infections. Clinicians often recommend Floxacillin for hospitalized patients exhibiting severe pneumonia or those with a history of antibiotic resistance.
Mechanism of Action and Pharmacokinetics of Floxacillin
Floxacillin operates by inhibiting bacterial cell wall synthesis. It binds specifically to penicillin-binding proteins (PBPs), which play a crucial role in the final stages of peptidoglycan cross-linking. This action leads to cell lysis and death of susceptible bacteria.
Floxacillin demonstrates effectiveness against a variety of gram-positive bacteria, particularly those resistant to penicillin. Its structure enhances stability against certain beta-lactamases, making it potent in treating infections caused by Staphylococcus aureus.
Pharmacokinetics of floxacillin reveals rapid absorption following parenteral administration. Plasma concentrations peak within one hour after an intravenous dose. The drug has a half-life of approximately 30 to 60 minutes, necessitating multiple doses for sustained effectiveness.
Floxacillin distributes well into body tissues and fluids, allowing effective penetration into sites of infection. Renal excretion is the primary elimination route, with about 80% of an administered dose being excreted unchanged in urine. Monitoring renal function is advisable in patients receiving prolonged therapy to avoid accumulation and potential toxicity.
Adjustments to dosing may be necessary for individuals with significantly impaired renal function to maintain therapeutic levels while minimizing side effects. Therefore, regular assessment of renal parameters and clinical response is recommended during treatment.
Side Effects and Contraindications of Floxacillin Treatment
Patients taking Floxacillin should be aware of potential side effects, which may include gastrointestinal disturbances such as nausea, vomiting, and diarrhea. Some individuals may experience allergic reactions, manifesting as rash, itching, or swelling. If you notice symptoms like difficulty breathing or swelling of the face and throat, seek medical attention immediately.
Common Side Effects
Other common side effects include headaches, dizziness, and fatigue. In rare cases, Floxacillin may cause more serious effects such as liver dysfunction, evidenced by jaundice or unusual fatigue. Regular liver function tests can help monitor this aspect of treatment. Be sure to discuss any persistent or severe symptoms with your healthcare provider.
Contraindications
Avoid Floxacillin if you have a known allergy to penicillin or any of its derivatives. Individuals with a history of renal dysfunction should also proceed with caution, as dosage adjustments may be necessary. Patients with specific gastrointestinal issues, such as colitis, should inform their healthcare provider before starting this antibiotic.
Always inform your doctor about your complete medical history and any other medications you are currently taking to prevent potential drug interactions. Regular follow-ups will ensure safe and effective treatment.
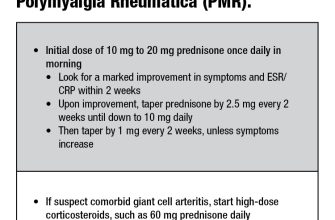
Guidelines for Prescribing and Dosage Adjustments of Floxacillin
For adult patients with uncomplicated infections, the standard dose of floxacillin is typically 250 mg to 500 mg every 6 hours. In cases of more severe infections, increase the dosage to 750 mg to 1 g every 6 hours. Adjustments are necessary for patients with renal impairment; reduce the dose according to creatinine clearance levels. For individuals with mild to moderate renal impairment (creatinine clearance 30-60 mL/min), consider a reduction to 50% of the normal dosage.
Monitor patients with severe renal impairment (creatinine clearance below 30 mL/min) closely. In such cases, a further reduction, potentially to one-third of the regular dose, may be required. Patients undergoing hemodialysis should receive floxacillin after dialysis sessions to maintain effective serum concentrations.
In pediatric cases, the dosing regimen is based on body weight. Administer floxacillin at 25 mg/kg to 50 mg/kg every 6 hours for children who are over 1 month old, not to exceed 1.5 g per day. For those who are under 1 month, because of immature renal function, consult pediatric dosing guidelines.
Consider the patient’s clinical response, and adjust dosages accordingly. Regularly assess for signs of effectiveness or adverse reactions to determine if further modifications are necessary. Always review any concurrent medications that may interact with floxacillin, especially those that affect renal clearance.
Consult local guidelines for treatment of specific infections, as resistance patterns can vary. For infections caused by penicillin-sensitive organisms, floxacillin is an excellent choice due to its activity against various staphylococcal and streptococcal species.
Regular blood samples may be recommended for patients on prolonged therapy to monitor levels, particularly in those with altered pharmacokinetics. Encourage patients to report any unusual symptoms, such as rashes or gastrointestinal disturbances, as these may indicate adverse effects requiring prompt intervention.